By Dr. Ernst Eiselen
Human skin is an ultra-sophisticated organ when it comes to protection against the physical and biological hostile world we all live in. A sophisticated laminated structure with temperature regulating dynamic cell and fibre barries cushioned on a comfortable bed of insulating fat, skin is a really smart protective barrier system for humans.
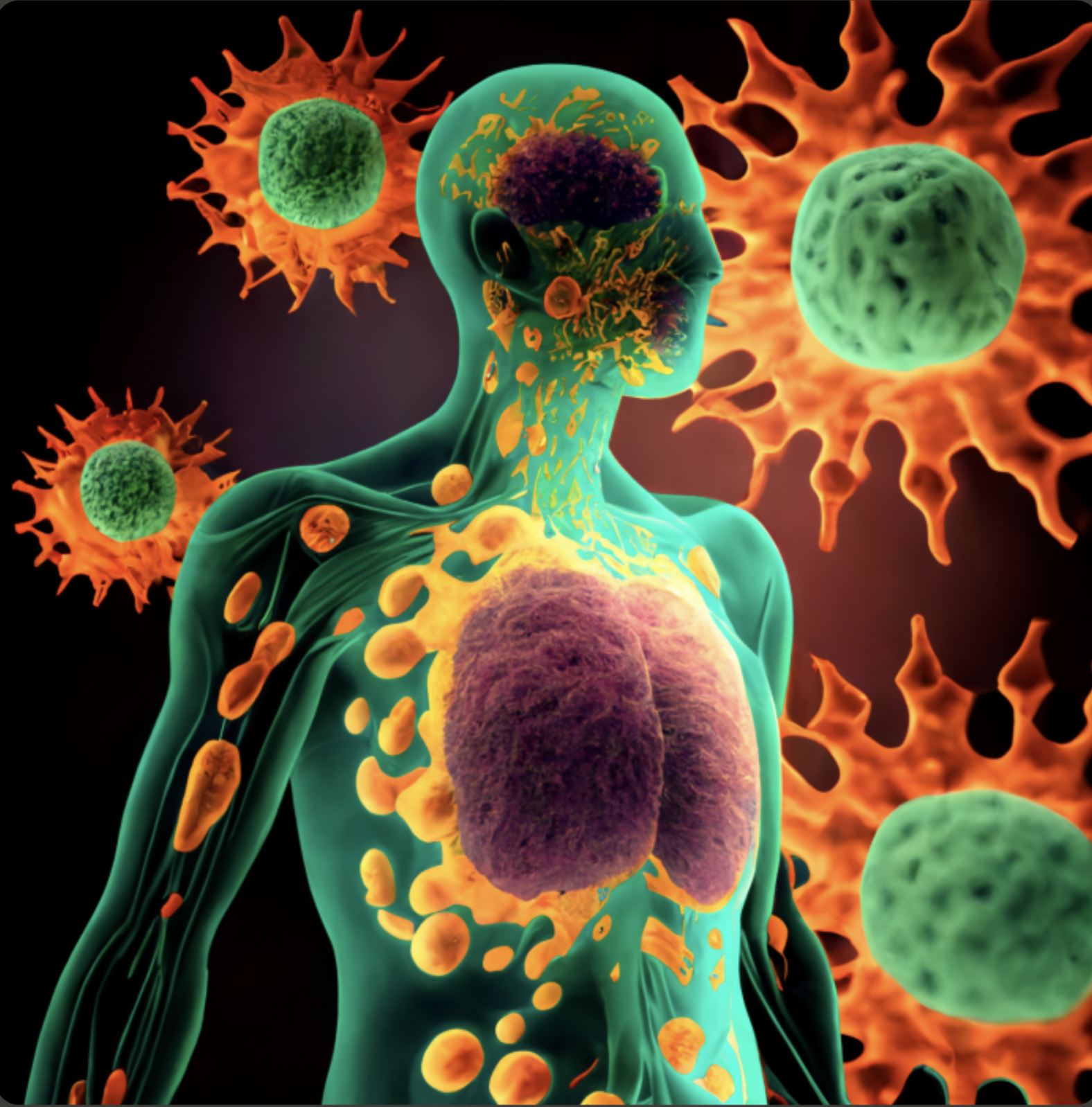
The excellent physical barrier is backed up by a skin associated lymphoid system, which connects the skin with all other elements of the immune system that serves the rest of the body to protect against infection, toxins and cancer. The immune system of our skin also has means of suppressing autoimmunity and does so effectively. Naturally, when this system malfunctions, one will see on of the many well described skin conditions such as psoriasis or lupus amongst others.
The physical barrier is best kept in shape by ensuring that the integrity of all layers and elements contained in the skin are kept healthy by providing optimal skin nutrition and water.
Human skin is constantly exposed to a variety of pathogens. Bacteria, viruses, yeast and fungi.
It reacts through the process called inflammation when a variety of the immune cells that are either already present at the site, or are called there by the reaction, get together to mount a range of protective responses. Inter-cellular communication is how they cooperate and make use of other information sources like those provided by the friendly micro-organisms of the skin, the keratinocytes and even nerve cells.
The immune system in the skin actively learns from these reactions and is then able to respond quicker and more efficiently when challenged again by any threats that have been met before. Every single distinct anatomical structure in the skin, from all cell types to the vascular bed and the lymphatic pathways, all play a role in the protection.
As in the rest of the body, there are elements that provide general protection also known as the innate immune system, and other specific elements called adaptive, as they are able to adjust to specific new or changing challenges. The cells involved in this process are the epidermal dendritic Langerhans cells and Keratinocytes. The dermis is equally well armed with Dermal dendritic cells, lymphocytes: T cells, B cells, natural killer (NK) cells, Eosinophils and Mast cells. Each has a specific role and are found throughout other organs in the body where they may look a little different, but function in the same way.
Skin has a collection of microorganisms known collectively as the skin microbiome, just as the good micro-organisms in our gut are increasingly being recognised as having very important functions in our general immune system. The skin is unique in our organ systems in that it has a fully-fledged defence system modelled in parallel to the greater immune system. It has intimate contact with the “greater” immune system by constant trafficking of immune cells to and from the lymphoid system and blood circulation.
Just as the gut is the front line for all we take in by mouth, so the skin is the true front line of defence against hostile and harmful elements in the world outside of our bodies.
Much research has shown the vital importance of maintaining good gut health for the sake of our ability to fight off or prevent diseases with which we are in contact from time to time.
It is very interesting to know that Vitamin A plays a pivotal role in the development and maintenance of the immune system. Extensive scientific research over decades shows this very clearly.
Our normal skin cells are generally thought to be structural in nature, forming the dynamic layer that gets changed every 40 to 60 days. Not so. They are clever detectors of molecules on disease causing organisms we call pathogens. They are then able to set off inflammatory reactions, which draw in the immune cells that can physically attack and remove the offenders. It is a very effective early warning system.
Keratinocytes have at least four different groups of molecules that act as messangerss to call the T and B cells of the immune system.
Macrophages – cells that can swallow and kill micro-organisms, are called to action.
These are all part of the innate defence system that do not depend primarily on memory of past contact with foreign molecules to act against them, but can tell foreign cells apart from the skin’s own.
The dendritic cells in the epidermis called Langerhans cells and those in the dermis have innate and adaptive responses to directly kill viruses and contain them or to examine and remember the foreign invaders before handing them over to other cells to kill them.
The third very important family of cells are called Natural Killer cells. They can destroy infected and cancer cells. They get chemical messages which program them into action. These wonderful molecules form the vocabulary of the immune system that allows cells to communicate with each other in very sophisticated and subtle ways. It is a highly evolved and very old system. The Complement System is a good example of this.
The Complement System and natural killer cells are important components of the innate immune system in the skin. These systems provide an immediate response to foreign pathogens and tissue injury. They play critical roles in detecting and eliminating infectious agents, as well as contributing to overall immune system function.
The Complement System is a complex system of proteins that is activated in response to infection or tissue injury. It consists of more than 30 proteins that are synthesized by the liver, macrophages, and other cells within the body., including skin cells. The skin cells that produce complement proteins include keratinocytes, Langerhans cells, melanocytes, and fibroblasts. These cells synthesize and secrete complement proteins that are involved in innate immune responses against pathogens and tissue damage. The Complement system is an important part of the host defence system on the skin, and its activation helps to initiate phagocytosis, inflammation, and tissue repair.
The Complement system is essential for the maintenance of skin homeostasis and protection against infection, suggesting that these cells are critical for the proper functioning of the skin’s immune system. The detail of this system is complex and function by initiating the so called “complement cascade “
The cascade is initiated by three different pathways: the classical pathway, the lectin pathway, and the alternative pathway. Each of these pathways result in phagocytosis of pathogens by macrophages and neutrophils. Some complement proteins like C3a and C5a are both anaphylatoxins, which can cause inflammation and recruit immune cells to the site of infection. The Complement system also plays a role in the clearance of immune complexes and apoptotic cells. These are cells that died by a programmed cell death.
Natural killer (NK) cells are a type of lymphocyte that can detect and kill infected or transformed cells in the body. NK cells are important in the control of viral infections and the prevention of tumour formation. NK cells are activated by a variety of signals.
Once activated, NK cells release special cell signals called perforin and granzyme molecules, which induce apoptosis (programmed cell death) in target cells. NK cells also release cytokines, such as interferon-gamma, which can further activate the immune response.
NK cell function is controlled by an array of receptors. These include inhibitory receptors and activating receptors. The inhibitory receptors recognize self-antigens and prevent NK cell activation against healthy, own cells. However, when an NK cell encounters an infected or transformed cell, the expression of self-antigens may be altered, leading to reduced inhibitory signalling and increased activation of the NK cell. To attack and remove the abnormal cells The activating receptors recognise stress-induced ligands (molecules that fit on cell receptors) or viral antigens on target cells, leading to NK cell activation and killing of the abnormal cells.
The Mast cells are sometimes referred to as the allergy cells in the skin. They are certainly responsible for the redness, itching and swelling of the skin during reactions, yet the reaction is a means of protecting against toxins, venom and chemicals. The problem with them is when a person has developed an allergy to a substance, the Mast cells can be coaxed into over-reaction leading to the allergic reactions we all know well. The worst of these reactions can be life threatening and is known as anaphylaxis.
One can write several chapters about the white blood cells called lymphocytes and neutrophils which form part of the more adaptive immune system. Adaptive here means that the cells develop a specific memory for a pathogen which then arms the system to launch a full attack during any future encounters. The best examples would be the organisms to which we have managed to make excellent vaccines like measles, mumps, diphtheria, whooping cough, cholera and typhoid.
The description of the skin’s protective characteristics allows us to appreciate what we can do to maintain the best protection to help the skin to protect us optimally.
The best course is to keep the structure of the skin healthy by having a good diet, protective clothing and sun protective creams, providing advanced vitamin skin nutrition and protecting the skin microbiome.
Lifetime supplementation of Vitamin A , C and E forms the basis of advanced skin nutrition.
Vitamin A is a critical molecule to maintain the health of cells in the skin immune system.
A constant supply of vitamin A from birth is vital to the whole of the system.
The epidermis contains a number of these cells and is literally last in line to get vitamin A supply from the body. Excessive sun exposure kills off vitamin A molecules, which leaves the epidermis in a net deficit very often. Not only does this leave the epidermal cells in a predicament, but it also leaves the other cells dealing with immunity in a similar state.
Unless humans change in the most fundamental genetic way imaginable, this will never change. There is a clear, dynamic connection between the skin immune system and the systemic immune system. This also emphasises the need for a gut-healthy diet when choosing food to eat. Equally, it is just as important to provide the skin with a balanced healthy “diet” in the form of topical Vitamin A ably supported by other vitamins, smart peptides and moisture to keep it as healthy and strong as possible.
Well established scientific facts provide excellent guidance for the best actions to enable skin to provide the best possible defences.
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6162863/
- https://dermnetnz.org/topics/skin-immune-system
- Kim, H.J., et al. (2017). The Skin Immune System: An Essential Component of Health. International Journal of Molecular Sciences, 18(10), 2117.
- Kim, H.E., et al. (2015). Skin Immunology and Immunodermatology. Clinics in Dermatology, 33(3), 292-301.
- Wollina, U., & Boms, S. (2013). The Skin Immune System in Health and Disease. The Open Dermatology Journal, 7, 1-9.
- Sugiura, K., et al. (2007). Skin Immunity and Its Regulation. International Journal of Molecular Sciences, 8(3), 265-287.
- Schafer, J.A., et al. (2010). The Skin Immune System: A Comprehensive Review. International Journal of Molecular Sciences, 11(4), 1553-1574.